Partial or complete narrowing of the subglottic area may be congenital or acquired. The problem is rare and challenging, affecting soft tissue and cartilage support.
Iatrogenic injuries cause most of the problems seen. Often, subglottic stenosis has an insidious onset, and early manifestations are usually mistaken for other disorders (eg, asthma, bronchitis).
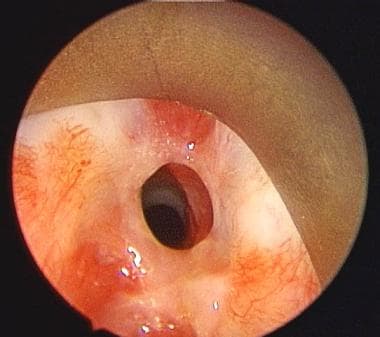
An image depicting subglottic stenosis can be seen below.
Preoperative view of subglottic stenosis via an endoscopic approach.
Congenital stenosis has two main types, membranous and cartilaginous.
In membranous stenosis, fibrous soft tissue thickening is caused by increased connective tissue or hyperplastic dilated mucus glands with absence of inflammation.
Membranous stenosis is usually circumferential and may extend upward to include the true vocal folds.
In cartilaginous stenosis, a thickening or deformity of the cricoid cartilage most commonly occurs, causing a shelflike plate of cartilage and leaving a small posterior opening.
Cartilaginous stenosis is less common than membranous stenosis.
Acquired subglottic stenosis is secondary to localized trauma to subglottic structures. Usually, injury is caused by endotracheal intubation or high tracheostomy tube placement. If irritation persists, the original edema and inflammation progress to ulceration and granulation tissue formation. This may or may not involve chondritis with destruction of the underlying cricoid cartilage and loss of framework support.
When the source of irritation is removed, healing occurs with fibroblast proliferation, scar formation, and contracture, leading to stenosis or complete occlusion of the airway.
Presentation:
Adults with mild congenital stenosis are usually asymptomatic, and they are diagnosed after a difficult intubation or while undergoing endoscopy for other reasons.
Patients with acquired stenosis are diagnosed from a few days to 10 years or more following initial injury. The majority of cases are diagnosed within a year. Symptoms include the following:
* Dyspnea (may be on exertion or with rest, depending on severity of stenosis)
* Stridor
* Hoarseness
* Brassy cough
* Recurrent pneumonitis
* Cyanosis
Many patients would have been diagnosed with asthma and recurrent bronchitis prior to discovery of stenosis. A high index of suspicion is warranted with the onset of respiratory symptoms following intubation, regardless of the duration of intubation.
Source:medscape
No comments:
Post a Comment